The National Council on Aging reports that one third of all chronically ill people say they leave a doctor's office or hospital feeling confused about what they should do to continue their care; 44 percent of people (aged 44 and older) with chronic conditions want their doctors to spend more time talking with them; and 57 percent report that their healthcare providers have not asked whether they have help to manage their conditions at home.
Most of these concerns arise from the fragmented nature of health care delivery in America and the fact that there's often a gap, a disconnect in the amount of digital health information and the exchange of data among providers, patients and caregivers. How often do patients go in for routine tests but never receive a call about their results, good or bad? Why do some patients wait hours to see a physician, only to spend 15 minutes in the exam room and not have all of their concerns heard or addressed?
The healthcare system today is so taxed that physicians often feel pressure to see as many patients as possible, in the shortest amount of time. Though it's a sad state of affairs, the impact can be minimized through today's increasing reliance by society on mobile devices, which can lead to better patient-provider interactions. mHealth, participatory health and participatory medicine are just a few terms that address this new area of healthcare but what do they all mean?
Understanding mHealth
According to the mHealth Initiative, only one year ago, many people didn’t know the meaning of the term "mHealth." Now more and more individuals are familiar with the term (also written as m-health or sometimes mobile health), a recent moniker for medical and public health practice supported by mobile devices.With the lofty, ambitious and admirable goal of connecting providers, patients, payers, and others came a complement to this endeavor, the idea of better communication in healthcare through participatory health.
Defining Participatory Health
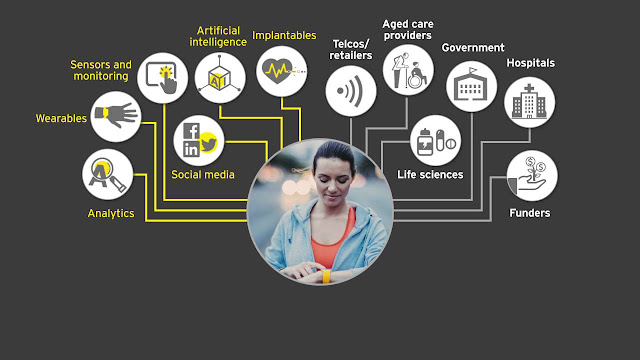
Most experts define participatory health as a partnership between patients and providers and trusted experts, one in which participation is enabled and enhanced by technology such as the Internet and mobile health platforms.Participatory health is also sometimes referred to as participatory medicine, a movement in which networked patients shift from being mere passengers to responsible drivers of their own health, and in which providers encourage and value them as full partners, according to the Society for Participatory Medicine.
The Need for Participatory Health
In a September 2009 report prepared for the California Healthcare Foundation, "Participatory Health: Online and Mobile Tools Help Chronically Ill Manage Their Care," Jane Sarasohn-Kahn, M.A., M.H.S.A, Think-Health, includes the following quote that speaks volumes about the state of healthcare today and the need for participatory health:"In our country, patients are the most under-utilized resource, and they have the most at stake. They want to be involved and they can be involved. Their participation will lead to better medical outcomes at lower costs with dramatically higher patient/customer satisfaction." - Charles Safran, M.D., President, American Medical Informatics Association in testimony before the Subcommittee on Health of the House Committee On Ways and Means, June 17, 2004
To this end, companies like Healthetreatment strive to enable individuals to share health and wellness knowledge so that others diagnosed with the same or similar conditions can learn from their experiences. Simply put, the site is creating a catalog of health conditions, symptoms and treatments compiled by real people.
According to Mike Bennett, the founder of Healthetreatment, user-generated health information is more robust and more current than existing medical resources. The key to being current and comprehensive, in his view, is to keep people coming to the website to provide the latest information on their condition.